Child Health Efforts Gain Momentum
A 2- day consultative meeting aimed at strengthening integrated child health services through the Primary Health Care (PHC) framework has taken place in Freetown.
Attended by over 55 participants drawn from government ministries, health agencies, and development partners, it was facilitated by the World Health Organization (WHO) and supported by United Nations Children Emergency Fund (UNICEF), CHAMPS, and other technical partners.
The dialogue focused on streamlining resources and expanding critical services such as district-level immunization, digital Integrated Management of Childhood Illnesses (dIMNCI), and specialized child care.
The meeting also reviewed Sierra Leone’s national mini-workplan from a recent regional consultation, ensuring alignment with WHO’s new Regional Framework for Strengthening Integrated Child Health Services. It also produced strong alignment on priorities, with particular emphasis on scaling the district initiated IMNCI approach (dIMNCI) and advancing early childhood development (ECD) initiatives.
The consensus signals a roadmap for integrated financing. By embedding child health within the broader PHC system, the government aims to streamline procurement processes, unify service delivery, and unlock critical donor funding aligned with the Sustainable Development Goals (SDGs).
This strategic alignment promises to reduce redundant programs and establish a transparent cost structure, enabling districts to secure necessary funding for vaccines, essential medicines, and maternal and child health services.
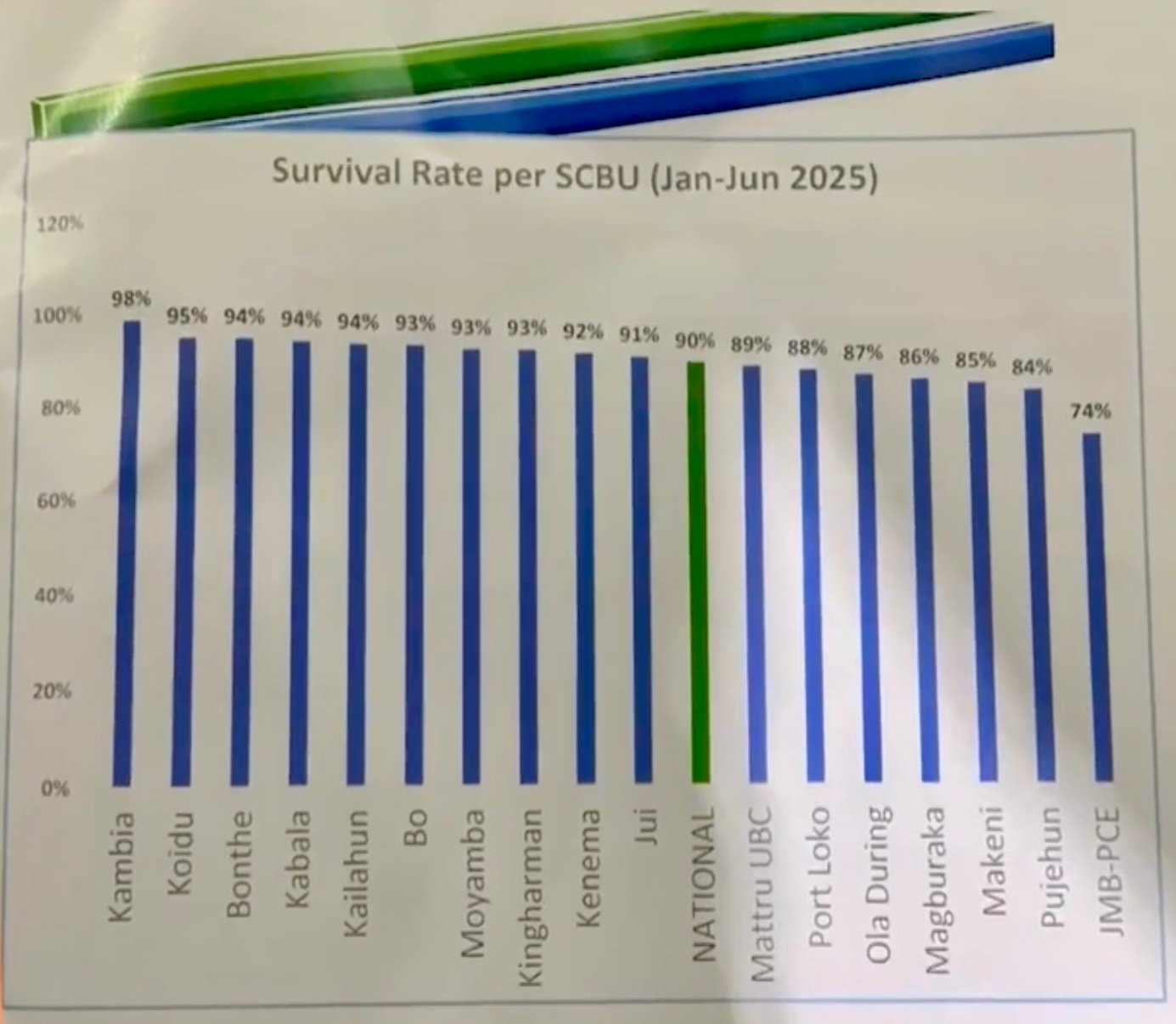
The proposed scaling of dIMNCI—an integrated approach to managing childhood illnesses will require substantial investment in health worker training, supervision, and supply chain infrastructure. The projected long-term benefits include reduced hospitalization rates, improved child survival, and a more productive future workforce. These measurable outcomes are particularly attractive to impact investors and development banks evaluating health-sector portfolios.
Moreover, prioritizing Early Childhood Development (ECD) opens the door for multi-sector financing. Strategic investments in nutrition, caregiver education, and cognitive stimulation programs can attract grant funding and blended finance models that integrate health with education and social protection initiatives, diversifying revenue streams for implementing agencies.
However, the success of this initiative hinges on securing multi-year funding commitments. Reliance on short-term grants risks disruption if domestic budgets or donor priorities shift. Addressing capacity gaps at district and facility levels is also essential to ensure smooth rollout—requiring robust supervision, reliable data systems, and a stable supply chain to prevent service bottlenecks.
Real-time monitoring is equally critical. A comprehensive results framework must track improvements in child morbidity, growth indicators, and developmental milestones—key metrics that will help sustain donor and government support.
This engagement positions the government to treat child health as a core component of PHC rather than a stand-alone program. If collaboration efforts translate into fully funded, scalable pilot projects particularly for dIMNCI expansion and ECD, Sierra Leone could create a model for West Africa. Such a model would appeal to international lenders and philanthropic organizations seeking integrated, outcomes-based health investments that align with SDGs.
By prioritizing and establishing a dedicated long-term budget line for integrated child health within the PHC framework, alongside a phased implementation plan for scaling up dIMNCI and ECD programs, Sierra Leone can build a sustainable platform.
Complementing this with a results-based financing framework will help unlock both public and private capital as milestones are achieved, ensuring a durable impact beyond the current consultative cycle.
This concerted effort will not only improve child health outcomes but also strengthen Sierra Leone’s economic outlook by investing in its future workforce.
While this meeting focused on integration and technical planning, it is part of a wider health sector momentum. In March 2025, Sierra Leone also launched its Collaborative Advocacy Action Plan (CAAP) a separate but complementary initiative designed to align women’s, children’s, and adolescents’ health commitments with national and global priorities.
Together, these efforts signal a coordinated national push to strengthen health systems, improve service delivery, and position Sierra Leone as a regional leader in integrated health investment.